My Mastectomy Recovery (Drains, Expanders, Infection, & more)
Written on April 5, 2022
The topic I had the most questions about, aside from how I prepared for the surgery, was just about what the mastectomy recovery process was like. I don’t even know where to start, so I am just listing off big parts of the process that I remember.
Having a support system
My mastectomy recovery could never have been so relatively ‘easy’ without my support system of friends and family (especially my husband and mother, who were literally getting their hands bloody helping me on a daily basis), and the fortunate position I was in to have a job that provided me with paid sick leave and healthcare. I do not know how women go through this alone or who don’t have supportive jobs, or even who have kids depending on them. Those women are truly extraordinary. Finally, I know that my recovery would never have been so smooth without the insanely incredible care I was given by the staff at Memorial Sloan Kettering (‘MSK’). Those people are miracle workers.
Going into the surgery
I am not a cryer. With the exception of physical pain, I almost never cry. However, I was hysterically crying daily leading up to the surgery. I’m talking, tears of utter and total anxiety. Everyone I speak to who is going in for this surgery since mine has told me they’re a ‘basket case’, to which I respond: I was the exact same way. It’s totally normal. In fact, one doctor told me (while I was in tears about to get my anesthesia) “if you weren’t this nervous, I think I’d be worried.”.... All I can say is: for me, the anxiety leading up to the surgery was the absolute worst part of the entire thing.
Waking up from the surgery
All I remember was that my first words were “Is it over? Am I alive?” to the nurse. Then I asked for my husband and immediately fell asleep. I stayed in the hospital for about 24 hours while they monitored me, and then was able to leave the next day in the early afternoon (~30 hours after I arrived). During that time, I had a lot of visits from doctors, the surgeon, the nurse, and even a physical therapist who taught me some exercises I should do on my own at home to regain use of my arms. I certainly wasn’t able to do much with my arms (aka nothing at all) for the first day.
Pain
I didn’t feel much pain at all waking up, and I think that’s because of the “Nerve Block” I had. Nerve blocks were optional at MSK, the hospital where I had my procedure. They start by telling you all the scary risks of getting one, but then tell you the goal is to limit how much pain you feel for the first 24-48 hours, and they also told me that >95% of people choose to get the nerve block. So I did. And man am I glad I did. The nerve block made it so this surgery really wasn’t so bad at all.
They gave me a ton of pain meds (the strongest being oxy) and explained the different use-cases for each of the pain meds (one for tightness, one for sharp pain, and so on).
I think I was on oxy / narcotics for just 2-3 days after the surgery, and then switched to ibuprofen.
The annoying pain came in a week later, with the expanders (see below).
Drains / what are drains
Drains are something you’ll hear a lot about leading up to the surgery, but you won’t truly understand how annoying they are until you have them. And by the way - for side sleepers (like me), be prepared to not get a good night’s sleep until they’re out.
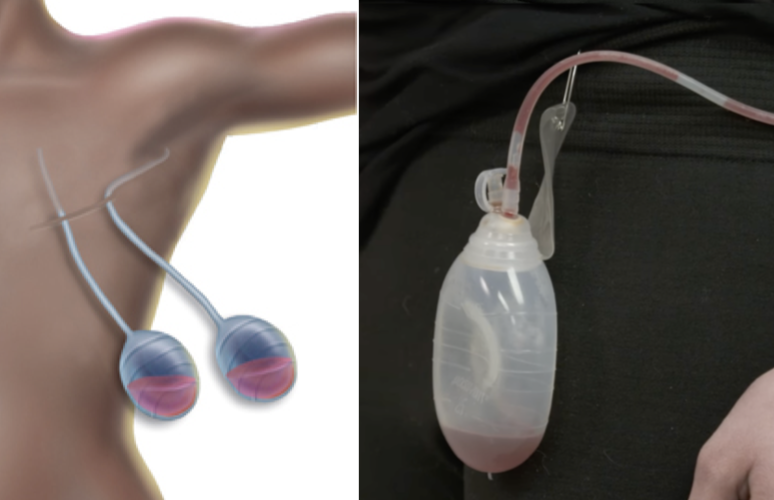
First: what are drains. From what I understand (remember, I’m not a doctor), drains are put into your body to collect and remove excess blood from the surgical site after the mastectomy. I had 2 on each side that essentially suctioned out blood from my chest and back areas. The blood gets drained into small suction cup things that then dangle at the end of long tubes (the tubes that stick out of your side).
My husband and I were taught how to empty the drains each morning and night – the nurse taught us in the hospital the day after surgery (click that link to see how it’s done). We would then have to measure how much blood was coming out, because once you get to a certain amount of blood (a low enough amount), you can go to the hospital and get that drain removed. I had 2 drains removed on day 8 after the surgery, and the other 2 removed on day 16. Here is a video of one of my favorite influencers getting her drains pulled out.
The only part of the drains that “hurt” me was when either something pulled (like a thread on my shirt got caught or the drain pulled down if I dropped it) and suddenly I’d feel a very sensitive part of my skin tugging — not good. Also, at the end, scabs started to form around the drain incision and those would constantly get caught on my shirt which hurt a lot.
Expanders / what are expanders
As I mentioned in another blog post, I was told I was not a candidate for “DTI” (direct to implant), where they can put the implants in during the same surgery as the mastectomy. Instead, when my mastectomy was done, I had ‘expanders’ put into me, which are expandable rubber things that essentially expand your skin / muscles / tissues to fit a new implant in (because they had cut off so much of my skin, they had to expand my chest to make way for implants). Here’s a picture I took of expanders that the nurse let me hold.
How expanders work: as I mentioned, the surgeon put the expander into my breast area after he took out all my tissue. They actually had the expanders filled already with 250cc of saline, so when I woke up from the mastectomy, I already had a TINY bit of volume in my chest area. After about 3 weeks from when my mastectomy was done, and once all of my scabs were healed / came off, I came into the doctor’s office 1-2x per week, where they would take a huge needle with 50cc of saline and would inject it through my skin into the expander (they used a magnet to find the right part of my chest to put the needle into). This sounds incredibly painful, but I lost almost all feeling on my chest, so I actually felt nothing each time except once when it hurt. Here is a video one of my favorite influencers posted of her expanders getting filled.
Once I was happy with the size of my chest (which, for me, was when I felt like it was the same size as I naturally had been), I stopped my expansions. I believe this was after my fifth expansion (some expansions were done with 70-100 cc).
In total, I had expanders for exactly 12 weeks (which is the amount of time that took place between my mastectomy and my reconstruction.)
There were 2 really bad things about expanders for me:
1) Expanders flipping: I guess because my skin is ‘loose’, or maybe because I move a ton in my sleep, my expanders decided to do acrobatics in my chest. My expanders were flipping almost every week, which meant they looked weird and they felt super uncomfortable. My doctor wasn’t concerned about this, but it just meant they had to flip them upside down at most visits, which hurt (imagine a doctor or PA getting on top of you and flipping a thing inside of your breast — ouch!)… The surgeon said he put extra ‘mesh sheeting’ in me during the reconstruction to make sure this wouldn’t happen with my permanent implants. Fortunately for most, I was told most people don’t experience expanders flipping often.
2) Pain: imagine I put two balloons inside your chest whose job was to expand your skin / tissue (and sometimes muscle). That would hurt, right? Yep. Expanders hurt A TON (much more than drains) for me for the first several weeks, but stopped hurting at the end.
My first shower
Oh my goodness was my first shower a memorable, horrible, and emotional experience. The first time I saw what I looked like in the mirror coming out of the mastectomy was 48 hours after surgery, when I was allowed to take a shower (using organic, perfume-free soap). My mom had come over to help me with my first shower in case I lost balance, but when I went to undress in the bathroom, I caught a small glimpse of my chest in the mirror (which had previously been covered with medical gauze, bandages, and a mastectomy bra), and I just started balling. Something about seeing how different it looked was just … emotional. I wish I had been a bit more prepared for that. So be warned.
Other than that, the first shower wasn’t so bad. I waited a week to wash my hair after my surgery because I couldn’t lift my arms enough to wash my hair, but that’s about all I remember as being worth noting.
Restrictions
So many restrictions!! Listen to your doctor for what yours are, but here were some of mine:
No lifting anything >5 pounds for 6 weeks
No alcohol for a few weeks (certainly not while I’m on narcotics) and no sex until at least 3-4 weeks
Must do physical therapy every day, five times each day (this adds up to a lot and is super tedious)
No deodorant or shaving my armpits until the drains are out (16 days) — so I used these wipes to wipe my armpits throughout each day.
No strenuous exercise (which for me meant I just was left with walking, or going up / down stairs) for 6 weeks
No ice or heat packs on the chest because I lost all feeling and could hurt myself
No driving until the drains were out
I wasn’t capable of lifting my arms above my head until around week 3. I was told by the nurse that I was way ahead of schedule compared to normal, but I think that’s because I’m young for the surgery / in good shape.
It hurt to sit up straight in a chair for more than 20 minutes until ~week 3. Otherwise, laying was most comfortable for me.
Walking / leaving the house
I was told that walking was good, but only to a certain extent (a couple thousand steps), because the more you walk, the longer your drains will be in (again, this is just what I was told by a nurse). For the first 2 days after surgery, I didn’t leave my house. By day 3, I was able to walk 1000 steps, but with a chaperone and with several stops (I would get out of breath or extremely light headed). Every 2 days after, I added a thousand steps, and by the end of week 3 or so, I was able to walk like ‘normal’.
By the way - getting in a car hurt for the first several weeks after, even with the seat belt cushion, because of the bumps on the road. I remember going to a friend’s home in Brooklyn and when we got to cobble stoned roads, I was in such pain I almost wanted to get out and walk (but knew I’d be out of breath before I made it — ha!)
Sleeping at the MSK Urgency Care unit with my infection / IV
Infection
Here’s where the only big “hiccup” during my recovery happened. One morning, fortuitously (and completely coincidentally) on the morning of an appointment I had with my doctor, about 8 days after surgery, I woke up vomiting. I was achey and could barely move. My mom convinced me to go to the doctor with her to my appointment (despite feeling too weak to get out of bed) and when I did, I learned that I had an infection in my breast. It was very early, but infections are one of the biggest “scary risks” that could happen during the post mastectomy period. So I was wheelchair’d immediately to the MSK Urgent Care building, and from there, I stayed in a room getting antibiotics through an IV for 3 days. It was miserable (the bed / room / food was not nearly as nice as the main MSK hospital) but I felt better almost immediately and the infection was gone by the time I left.
The lesson here: look in the mirror every single day (or have your partner look) and look for redness that is growing. The doctors / nurses will explain to you how to find a possible infection, but I’m so glad / lucky I caught mine before things got much worse. (Someone in the BRCA facebook group I’m a part of told me hers was so bad that they had to open her up, remove her expanders, let her heal, and then open uher up again and put in new expanders. I cannot even imagine going through that!)
So how did I get an infection? Most of the doctors and nurses I spoke with said it was almost definitely from a single germ finding its way onto the expander (or something like that) during the mastectomy, but you can never know. I slept on clean sheets and only wore clean clothing around my incisions, so I guess I’ll never know what the true cause was, but every doctor did say to me “it’s not your fault”. (The “doer” in me wanted to find the cause so I could avoid it from happening again, but oh well.)
Food
I’m copy-and-pasting from point #2 here: "
“When you can’t cook and it hurts to lift your arms to make a sandwich, having food sent to you is the best … NOTE: I recommend someone close to the ‘patient’ set up a “Meal train” (it’s free), which makes it easy for people to sign up for specific meals so that the person doesn’t get everything at once, and so that there’s variety. My sister-in-law, Jenn, set this up for me, and the meals were probably the ‘highlight’ of my entire first 2 weeks, and the main thing I’d look forward to each day. (Huge thank you to everyone who sent meals — you guys are the best.)”
I tried to eat mostly healthy since I was doing almost no physical exercise, but I will admit that I ate plenty of comfort food (babka, etc) alongside my meals. Nothing really to report on food outside of the fact that you need to be prepared to not cook or make food for at least 6 weeks, since I was told not to lift anything more than 5 pounds, and it took me ~8 weeks to have my arms fully feel back to normal.
I also had one daily ‘vice’ that I totally gave into (aka my husband put up with how much room in the fridge it took up!) which was a “Health Ade Kombucha” (pomegranate flavor)… Normally I wouldn’t splurge on a $5 drink every single day (that’s $150 of kombucha each month), but I was addicted and genuinely looked forward to it daily. If you can find something like that, you should! Especially if it’s healthy and makes you feel good :)
Clothing
During the 9 weeks between getting my drains out and having the reconstruction, finding outfits to wear wasn’t the easiest, especially for nice occasions. I didn’t always feel comfortable wearing something form fitting, mostly because the expanders (especially when flipped upside down) would show weird bumps on my chest due to the indents of the rubber. So I tended to just wear loose tops, or something form fitting with an infinity scarf that would cover my chest.
Taking time off
I was told by everyone who had been through this who I spoke with that I should take 2 weeks off from work. So I did, but by day 8, I was actually able to log back into work and work half-days for the 2nd week. Keep in mind, I was fully remote and my job required nothing physical (just working at a computer). I will admit that I worked from bed (thank you, Zoom backgrounds, for making this possible!)
What did I do all day during those 2 weeks? 1) Sleep, 2) watch TV / movies, 3) sleep, 4) eat, 5) sleeeeeeep. And of course, doctor appointments, which my mom accompanied me for (it’s so nice to have someone with you if you are lucky enough to have someone who can take the time off — in my case, my mom is retired and lived 15 mins away from the doctor.)
Appointments
As you’ll see in the “Expander” section above, I had to go to the doctor all the time. Ignore my infection for a moment — I probably went to MSK a total of 20 times between Jan 7th 2022 (my first pre-opp appointment ahead of the surgery) and April 6th 2022 (my one-week follow up post reconstruction). So I felt really fortunate that my husband and I were flexible enough to have booked an Airbnb to rent for 3 months that was right near the hospital. It took me just 12 minutes to get from home to the doctor, which meant I was able to take care of most appointments in 60-90 minutes from door to door.
I know I said it earlier in this post, but to reiterate once again: nothing I went through would have been nearly as smooth had it not been for the incredible work and brilliance of the staff (especially the doctors and nurses) at Memorial Sloan Kettering. Thank you, thank you, thank you.